Macular Holes
Let us answer a few very important questions about macular holes. What is the Macula? and why is having a hole in your macula a concern? How does a person know they have a macular hole? How do we diagnose this? How do we treat and manage a macular hole?
A macular hole occurs when there is any sort of break in the macula. This is so devastating because the macula is the small oval area where all of our sharp central vision comes from. Without the macula we would not be able to drive, read, see color and we would have no fine detail vision.
Symptoms:
Patients with a macular hole will often report blurry vision, black spots and or distorted vision. In general a macular hole will only affect your central vision leaving your peripheral or side vision unaffected.
Who is at risk:
macular holes are often related to aging processes so we are more likely to see them in patient over the age of 60.
Some of the most common causes of macular holes are:
– The vitreous sac in the back of the eye can overtime shrink and can pull on the macula.
-They can occur secondary to Diabetic eye disease
– High amounts of myopia (Nearsightedness) may lead to macular holes because the eye is very long in high myopics and can cause retinal stretching/ pulling on the macular area.
-A macular pucker also called a ‘epiretinal membrane’ occurs when scar tissue is formed on top of or surrounding the macula and can cause traction on the leading to the hole or the tissue itself which can cause blurred vision.
– traction between the vitreous and the macula
-A detached retina
-injury to the eye
Treatments
The cause of the macular hole will often determine the treatment. The most common treatment is a Vitrectomy. In this procedure the retinal specialist will remove the Vitreous gel which is often the cause of the pulling. It is then replaced with air and gas. The gas bubble pushes on the back of the eye where the macula is and helps push it back together. Negative effects of the vitrectomy is the development of a cataract quickly after, risk of infection, no air travel for months.
Intravitreal injections are another form of treatment. These injections use a drug Ocriplasm ( jetrea) to help dissolve the traction between the vitreous and the macula. There are some limitations as it works best on small holes, patients who have not had cataract surgery and has no effect on epiretinal membranes.
Monitoring
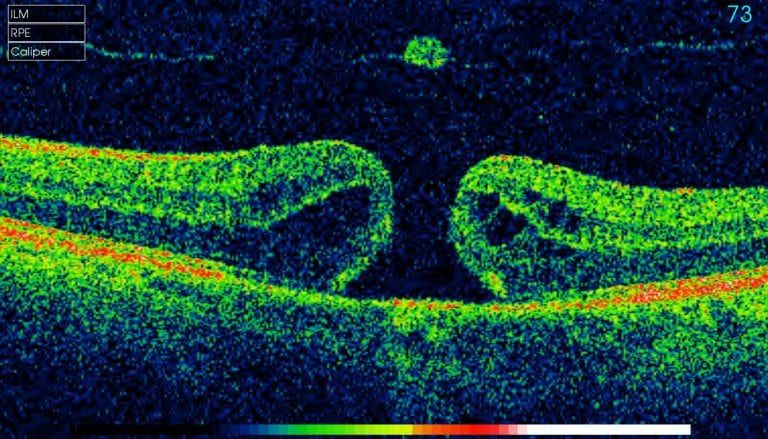
Your retinal specialist or optometrist will want to have regular followups with any patient who has a retinal hole or partial retinal hole. Vision is monitored, and retinal mapping is done by an optical coherence tomography or OCT. An OCT Images all of the retinal layers below the surface of the retina and helps to determine when a referral and or treatment is necessary.
Patients being monitored for a macular hole or other central retinal diseases are often given a simple take home test and are to return to clinic if there are any changes.
There are some cases where a macular hole will resolve without surgical intervention, however most cases of macular holes do not repair on their own. It is therefore important to have them assessed by a retinal specialist once they are diagnosed or monitored by your optometrist. Because there is also a greater risk (approx. 10%) of developing a macular hole in your other eye once you have had one, it is important to continue with routine eye exams even after you have had a treatment or resolution of the hole.
-Dr. Alanna Adams












